North Cypress: 281-890-7444
The Woodlands: 281-363-2777
FAX: 281-890-0030
HIPAA email: drsingh@eyeoftx.com
CORNEAL TRANSPLANTS
The cornea is the clear tissue in front of the iris (the iris is the colored portion of the eye); the cornea is the window through which we see the world. Thus, the clarity, health, and smoothness of the cornea play a major role in determining the quality of our vision.
When the corneal health or clarity is compromised, a full- or partial corneal transplant may be an option to restore corneal transparency and function, thus restoring vision.
One common reason for needing a corneal transplant is a corneal scar that interferes with a patient's vision, such as from a trauma, infection or in some cases from a hereditary condition such as a dystrophy or keratoconus. Other reasons for corneal transplantation include failures of the mechanisms of the cornea naturally in place to keep the cornea clear, such as with Fuch's dystrophy.
A corneal transplant involves removing some or all (scarred or non-functioning) layers of the cornea, and replacing that damaged tissue with healthy corneal tissue from an organ donor.
Penetrating Keratoplasty (PKP)
Penetrating keratoplasty is the original approved corneal transplantation surgical method, and its history dates back over 100 years. Until recently, the majority of all corneal transplants in the United States were PK procedures. A PK involves cutting a circle to remove the full thickness of the cornea, (generally the central 7.0 mm – 8.5 mm diameter), and replacing that with a corneal button of donor tissue. The new (donor) cornea is sewn onto the host with usually about a dozen very fine 11.0 microfilament sutures.
Deep Anterior Lamellar Corneal Transplant (DALK)
Lamellar keratoplasty is a surgical procedure in which only a layer in the front of the patient’s cornea (anterior) is removed and replaced. In this manner, the back (posterior) layers of the cornea remain intact.
By not transplanting the inner endothelial layer of the cornea, it is hoped to reduce the risk of rejection of the cornea. Additionally, visual rehabilitation may occur more rapidly and the long-term success of the cornea is increased.
Dr. Singh is one of only a few corneal transplant surgeons routinely performing this technique, and he was the 1st surgeon in Houston to perform a variant of his technique known as the maximal depth (or Big Bubble) technique. This variant technique achieves a smoother interface and visual potential is increased.
Deep Anterior Lamellar Keratoplasty is suitable only for those patients with a corneal disease that involves only the anterior or stromal portion of the cornea. Examples of corneal diseases that may be amenable to DALK include keratoconus and corneal scars. Dr. Singh will determine if this is a suitable option with a clinical evaluation.
Endothelial Corneal Transplant (DSAEK + DMEK)
This is a great option for individuals with conditions such as Fuch's dystrophy, in which the inner (posterior) layer of the cornea fails to function properly and leads to corneal edema and clouding.
With an endothelial keratoplasty, the healthy anterior part of a patient’s cornea is retained while their diseased corneal endothelium is replaced with healthy donor tissue through a small incision. No sutures are needed in this procedure to hold the donor cornea is place, and only a few sutures are placed at the surgical incisions. These sutures are generally removed much earlier than with other corneal transplantation techniques, most often from 2 to 6 weeks after the surgery.
One of the exciting aspects to these newer surgical procedures (and there are several) is that the recipient’s cornea remains structurally intact and resistant to injury. Additionally, the visual rehabilitation is much faster and occurs in 2 to 3 months as compared to 12 to 18 months for the traditional PK.
The DSAEK procedure replaces the inner-most 50 micrometers of the diseased cornea and is the original endothelial transplant technique. The newer technique is the DMEK procedure, which involves an even thinner sheet of donor tissue, approximately 5 - 10 micrometers thick. The DMEK procedure provides faster and better vision rehabilitation, but it requires exceptional experience and skill, and Dr. Singh is one of the few corneal specialists capable of performing this technique.
Artificial (Synthetic) Corneal Transplant
An artificial corneal transplant is a technique used to rehabilitate those patients who have previously undergone a penetrating keratoplasty (PK), but whose corneal transplant has failed and the prognosis for another corneal transplant is poor. These include cases such as a severely vascularized cornea where the chance of rejection is high, or patients who have previously had 2 or more corneal transplants that failed due to where rejection.
This technique involves securing an inert plastic disc on a carrier donor cornea that is then sewn onto the patient’s cornea after the previous damaged tissue is removed. This surgery can be highly successful, and may be the only reasonable alternative for patients who are poor candidates for further successful corneal transplantations. This condition requires more care by the patient postoperatively, but may allow for a more rapid visual recovery.
If you have had a poor outcome from previous corneal transplantation, Dr, Singh can evaluate your candidacy for this new and exciting procedure.

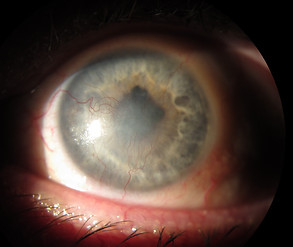
BEFORE PENETRATING KERATOPLASTY: PERFORATED CORNEAL SCAR (HOLE)

AFTER PENETRATING KERATOPLASTY (WITH A FEW SUTURES ALREADY REMOVED)

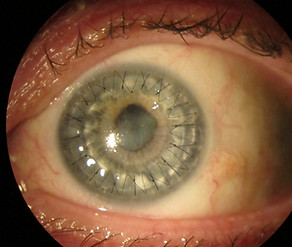
BEFORE PENETRATING KERATOPLASTY: CORNEAL ULCER

AFTER PENETRATING KERATOPLASTY
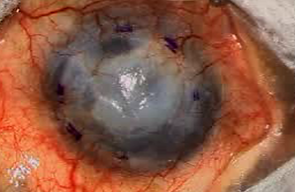
BEFORE DALK: CORNEAL SCARRING AND NEOVASCULARIZATION
AFTER DALK WITH SUTURES STILL IN PLACE
BEFORE SYNTHETIC CORNEA: CORNEAL GRAFT FAILURE
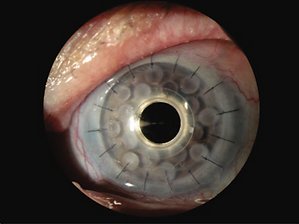
AFTER SYNTHETIC CORNEA
